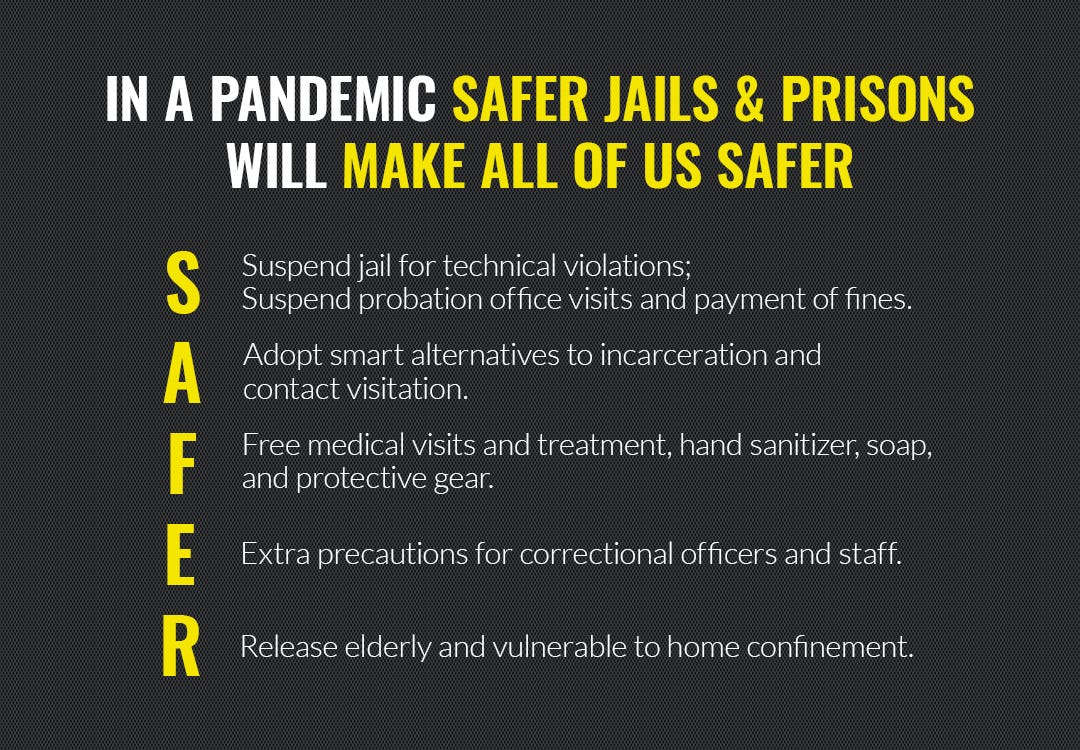
THE SAFER PLAN: PREVENTING THE SPREAD OF COMMUNICABLE DISEASE IN THE CRIMINAL JUSTICE SYSTEM
 Organizations endorsing SAFER plan
Organizations endorsing SAFER plan
Summary
CDC recommendations regarding COVID-19 are changing as our understanding of the spread, treatment, and management of the virus evolves. Many of the recommendations below are based on current CDC recommendations, but people responsible for protecting incarcerated and supervised populations should routinely monitor CDC updates and information from their local health departments — including county, city, and tribal health departments.
The United States incarcerates over 2.2 million people in prisons and jails, with many facilities operating well over capacity. Incarcerated persons have higher rates of underlying health issues than members of the general public, including higher rates of respiratory disease, heart disease, diabetes, obesity, HIV/AIDS, substance abuse, and other conditions that suppress immune response. The close conditions and lack of access to hygiene products in prisons and jails make these institutions especially susceptible to viral pandemics. Incarcerated persons often avoid seeking medical attention because of medical co-pays and lengthy wait times, which create a lag in identifying and treating conditions, leading to an increase in the severity and spread of illness. The spread of communicable viral disease in the United States constitutes a serious, heightened threat to the safety of incarcerated persons and correctional staff. The failure to contain and slow the spread of communicable viral disease in our jails and prisons creates a serious threat to the general public.
The United States has over 4 million people under some form of correctional control through community supervision (parole or probation). Communicable viral disease can also be spread by unnecessarily aggregating persons under community supervision in administrative offices, and by requiring them to adhere to conditions of supervision that require travel and interfere with recommended social distancing and quarantine protocols.
With that in mind, we’ve created the SAFER plan.
The following experts’ input, guidance, and publications were critical in developing the SAFER Plan:
- Craig Haney, PhD, JD; Conditions of Confinement and Psychology Expert and Professor at University of California, Santa Cruz
- Vincent Schiraldi, MSW; Senior Research Scientist at Columbia University’s Justice Lab and former Commissioner of New York City Probation.
- Mark Stern, MD, MPH; Correctional Health Care Specialist at University of Washington
- Alysse Wurcel, MD, MS; Geographic Medicine and Infectious Diseases Expert at Tufts Medical Center
The following groups also helped collaborate on the plan:
- Experts who have been directly impacted by the criminal justice system, including formerly incarcerated people and family members of those who have been impacted.
- Correctional officers and administrators
- Probation and parole officers
- American Conservative Union
- Americans for Prosperity
- Cut50
- Due Process Institute
- Faith and Freedom Coalition
- FAMM
- FreedomWorks
- Justice Action Network
- National Alliance on Mental Illness
- National Urban League
- R Street Institute
- Right on Crime
Here is the full list of recommendations contained with in the plan.
Legal Visitation / Alternatives to Physical Visitation
States and counties within the United States (and some countries, such as Italy) have suspended visitation into jails and prisons to slow the spread of COVID-19. While the importance of protecting communities from COVID-19 — and in this case, people behind bars and under supervision — is paramount, it is essential that the measures taken are the least harmful to the people they seek to protect. While suspension of physical visitation may be necessary to contain or slow the spread of the virus, measures such as suspension of all visitation and programming (discussed below), have significant negative effects on people under correctional control and their families. For example, psychological distress and increased incidences of violence are documented effects of such measures. Further, loss of access to legal rights, education opportunities, faith services, mental/medical health, and substance abuse treatment is also evident when suspension of visitation extends to professionals and volunteers.
Recommendations
In facilities where physical visitation is suspended, retain access to (and increase as needed to make up for the loss of physical visits) non-contact legal visitation.
Implement, as appropriate and available, alternative methods of visitation — such as phone calls, video visitation, and electronic communication — for all types of visits (family, nonlegal professional visits, legal visits where non- contact visits are not accommodated etc).
Phone calls, electronic communication, and video visitation fees must be waived during this time. At the very least, these fees should be reduced, with a certain number per week of phone/video visits and/or electronic communications provided at no cost, to ensure that vital connections to family and communities are not severed.
Medical Copays and Waitlists for Medical Care
Incarcerated persons may be required to pay copays for medical care, disincentivizing them from requesting medical treatment. Further, medical treatment inside of facilities often requires lengthy wait times. During these wait times, people may unintentionally and unknowingly spread the virus to others.
Recommendations
Waive copays for medical visits, medications, and medical supplies for symptoms that may be related to COVID-19. Ensure that people most vulnerable to COVID-19, as defined by criteria determined by current public health recommendations, are seen quickly. Provide surgical masks to people exhibiting symptoms (such
as coughing and sneezing) while they await medical screening and care. Provide N-95 masks (or, if those are not available, any mask with an N, P, or R and a 95 or 100 designation; if none of those are available, provide a surgical mask) to staff working in close proximity to symptomatic patients. Follow current public health recommendations on appropriate precautions for staff and incarcerated persons working in jobs that impact the health of others in the institution, such as food preparation.
Hand Sanitizer Availability and Declassification as Contraband, Soap and Hygiene
One of the only methods proven to slow and prevent the spread of coronavirus is hand sanitizer — specifically, the kind with alcohol in it.
Recommendations
Make available to all incarcerated persons at no cost hand sanitizer approved for slowing and preventing the spread of coronavirus. Declassify as contraband hand sanitizer with alcohol. Allow correctional staff to carry personal size hand sanitizer.
Make available to all incarcerated persons and staff an ample supply of soap, at no cost. Remove barriers to good infection control and increase access to good hygiene protocols. Ensure all incarcerated persons have access to running water and soap and are informed of the need to wash hands thoroughly, even if they have access to gloves.
Cleaning and Disinfecting Shared Spaces
In addition to hand sanitizer, cleaning shared surfaces with approved cleaning solutions has also been recommended to slow or prevent the spread of the virus.
Recommendations
Increase the cleaning schedules of all shared spaces within the institutions and clean with solutions proven to kill the virus. Make available to or provide a schedule for the same cleaning within cells.
Jails and Courtrooms
The spread of communicable diseases is often even higher in jails than prisons. For example, the rate of tuberculosis (TB) is anywhere from 5 to 100 times higher in the incarcerated population than in outside communities, but almost all of the data show that jail rates of TB are even higher than prison rates of TB. This may have to do with poor screening practices in jail, but it may also have to do to the higher turnover in jail. Consequently, it is essential to take additional steps to prevent unnecessary pretrial incarceration and reduce crowded courtrooms.
Recommendations
Use alternatives to incarceration for pretrial defendants. Unless an individual is adjudicated as a risk to public safety, utilize alternatives, such as home confinement, instead of incarceration.
Allow telephonic and video appearances in courtrooms to slow the spread of the virus.
Request postponement, subject to constitutional requirements and required consent, of all nonessential court dates that cannot be accommodated remotely.
Utilize Alternatives to Incarceration Consistent with Public Safety
Given the close living quarters, challenges with sanitation, and overburdened / undersupplied medical care systems in prisons and jails, all efforts must be made to reduce incarceration that does not implicate a threat to public safety. The necessity of social distancing and precautionary quarantines may result in significant disruptions to legal representation, severing of beneficial family connections, and loss of important programming — all of which can also impact the level of violence and overall safety within the institution — and every effort must be made to mitigate the negative effects of such disruptions for the over 2.2 million people behind bars.
Recommendations
Pretrial (defendants in custody/jail prior to conviction / adjudication): Identify and release people who have been detained pretrial and whose release would not constitute a serious threat to public safety. Release those persons to home arrest, electronic monitoring, or other conditions, as appropriate. Reduce the use of pretrial detention to the extent consistent with public safety and existing law.
Jail*(defendants in jail serving their sentence/postconviction): Identify persons currently incarcerated in jails who are within eight weeks of release and immediately release those persons to house arrest, electronic monitoring, or other measures necessary for the balance of the term of incarceration.
Prison* (defendants in prison serving their sentence/postconviction): Identify persons currently incarcerated who are within six months of release from incarceration and immediately release those persons from incarceration, implementing house arrest, electronic monitoring, or other measures as necessary for the balance of the term of incarceration.
Technical Violations* (defendants serving time in jail or prison for a technical violation of supervision / no new crime): Identify persons currently incarcerated due to a technical violation and immediately release those persons from incarceration, implementing house arrest, electronic monitoring, or other measures as necessary for the balance of the term of incarceration for the violation.
Compassionate Release*: Identify incarcerated persons who are elderly, immunocompromised, or meet the requirements for compassionate or elderly release. Expand and expedite the use of compassionate and elderly release and release those persons from incarceration, implementing house arrest, electronic monitoring, or other measures as necessary for the balance of the term of incarceration for the violation.
*Except that, this provision shall not apply to any person whose release is determined to constitute a serious threat to public safety, but such release shall not be unreasonably withheld.
Testing Kits, Protocols, and Identification/Mitigation of Symptoms
Multiple test protocols are necessary to ensure that the virus is contained.
Recommendations
Incarcerated Persons
Provide facilities with adequate testing kits to meet the needs for testing according to testing criteria established by the local health authority. Determine the extent of the crisis. Prioritize testing of vulnerable populations and people with symptoms.
In the event that testing kits are unavailable or scarce, test for symptoms of the virus, according to the most current public health recommendations. As of 3/15/2020, recommendations are to screen for the following: fever of 100 degrees, cough, shortness of breath, recent travel to a high-risk area, and exposure to someone who is symptomatic and under surveillance for COVID-19. If 2 out of 3 are present, prioritize COVID-19 testing and consider quarantine. These criteria should be updated to reflect evolving public health recommendations.
Visitors and Facility Staff
Anyone admitted into the facility must be tested to ensure that they are not bringing the virus into the facility. [See above for legal and family visitation recommendations.]
Staff reporting to work should be screened for symptoms of the virus according to the most current public health recommendations. Staff or visitors who screen positive must not enter the facility. The staff member should be advised to contact his or her health care provider for further advice, and the local health authority should be notified to assist the facility with managing the finding.
To anticipate reductions in staffing, facilities should consider liberalizing restrictions on overtime for current employees as well as considering sources of supplemental staff, such as retirees, and begin appropriate training. At the same time, facilities should consider ways of encouraging sick staff to not report to work, e.g. not penalizing staff who are absent after exhausting leave, or even expanding leave allowances.
Procedures for Suspected / Confirmed COVID-19 Cases
To prevent the spread of confirmed or likely COVID-19 cases, every possible effort must be made to separate out people with the virus from the rest of the incarcerated population. People with active symptoms or in need of treatment for the virus, should be safely transferred out of the facility as early as practicable to ensure they receive the care they need and prevent further spread.
Recommendations
[See above for recommendations related to safely releasing incarcerated persons who are not a threat to the community. ]
Create non-punitive quarantines for low-risk incarcerated persons who have likely or confirmed COVID-19. CDC recommends quarantine in negative pressure rooms. If negative pressure rooms are available, quarantine there. If negative pressure rooms are unavailable, consult with local health authorities and hospitals to determine appropriate alternative options.
Ensure that quarantine and isolation is non-punitive to encourage people to notify staff of potential symptoms as early as possible. Quarantine and isolation should have ample access to comfort, entertainment, and activity- related materials permitted in the pre-quarantine custody level. Every reasonable, available measure to mitigate the harmful psychological and physical effects of isolation should be taken to ensure that the quarantines do not create additional medical and mental health risks.
High-risk incarcerated persons (people whose age, history of illness, and active symptoms, increase the likelihood of necessary medical intervention), should be safely transferred to a medical facility that can accommodate them to ensure that they are appropriately quarantined and cared for.
No one should be incarcerated past their release date, even if quarantine is warranted. Confirmed cases requiring medical care must be coordinated with the appropriate hospital to facilitate the transfer from incarceration to medical supervision in a safe and timely manner. Individuals who are isolated for mild symptoms or quarantined as a precaution should be released with a plan for self-quarantine and both the supervision department and the local health department should be notified to ensure appropriate accommodations are in place.
Earned Time Credit, Programming, and Lockdowns
The need for social distancing, even in overcrowded facilities, will mandate changes to group settings, programming, and movement within the facility. Many of these programs have proven recidivism-reducing effects, as well as positive effects on safety within the institution. Consequently, while reducing programming and group activities may be essential to slowing the spread of the virus, all available alternatives must be utilized, with incentives remaining the same, to prevent the negative effects correlated with their cancellation. Similarly, every effort to mitigate the detrimental effects of movement restrictions and lockdowns must be made to avoid negative medical, mental, and behavioral consequences.
Recommendations
When possible, continue groups and programming that can accommodate the recommended 6-foot distance between participants. If unable to accommodate the required distancing protocols, institutions should
use whatever non-contact alternatives are available. This includes increasing remote classes, groups, and programming conducted by video, phone, or mail. It also includes cell-side visits from instructors, group facilitators, and faith leaders that are cleared to enter the facility and agree to abide by prevention guidelines consistent with current public health recommendations. During this time, earned time credit for participation in programming should still be accrued.
During lockdowns or periods of restricted movement, the facility should implement as many mitigating measures as possible, pursuant to the paramount goal of maintaining safety in the facility. These mitigating measures may include, but are not limited to: increasing entertainment time within the cell by allowing extended access to and use of television and radio; relaxing restrictions around the number of books and papers allowed inside of the cell; instituting cell-front phone calls, and; implementing cell-front programming and faith services.
Reducing Unnecessary Supervision (Parole and Probation)
More than double the number of people who are incarcerated are under some form of correction supervision, and subject to a number of conditions that prevent people under supervision from taking the recommended precautions to prevent and slow the spread of COVID-19. Limiting and reducing the use of unnecessary supervision and supervision conditions is essential to containing and mitigating the spread of the virus.
Recommendations
Identify persons who have successfully completed at least 3 years of supervision and transfer that person to administrative supervision or terminate supervision, as appropriate. Suspend fines and fees for formal, informal, and administrative supervision.
Technical Violations
In addition to reducing mandatory supervision meetings (to avoid group settings ripe for the spread of the virus), any/all non- essential confinement must be suspended.
Recommendations
Suspend incarceration for technical violations of supervision. Any/all confinement not essential to public safety must be suspended and alternatives must be enacted until the spread of the virus is adequately contained. Utilize alternative sanctions for technical violations. Use alternative sanctions for violations of the law that do not implicate public safety. No penalties shall be assessed for fines and fees not paid during this time.
Conditions of Supervision
Given the risk of spreading the virus in groups and gatherings, every effort must be made to reduce conditions of supervision that require travel and in-person meetings.
Recommendations
Suspend any/all conditions that require mandatory in-person meetings, including but not limited to office check-ins with supervision officers. Utilize phone check-ins or alternative methods instead.
Any in-person contact (such as drug testing) will only be conducted when the risks to both the supervising officer and the supervised person are mitigated; no supervision conditions will require the supervised person to travel to or attend group meetings that may put them at risk.
Discretionary groups and programming, such as alcoholics anonymous (AA) and grief support groups, should accommodate the recommended 6-foot distance between participants. If unable to accommodate the required distancing protocols, discretionary groups should use whatever non-contact alternatives are available (phone, video, or online groups).